July-August 2020 • Vol. 29/No. 4 237 Justin Omar Barredo, MSN, is Registered Nurse, Holy Name Medical Center, Teaneck, NJ. Room Assignments, Gender Identity, and Gender Expression: A Case Study on Caring for Transgender Patients Justin Omar Barredo
According to the 2015 U.S. Transgender Survey, 33% of transgender people reported
having at least one negative experi- ence in health care within the past year (James et al., 2016). This includ- ed refusal of treatment, verbal harassment, physical or sexual assault, or having to educate health- care personal on transgender care to receive proper treatment. As the number of people in the United States who identify as transgender has doubled to 1.4 million from a decade ago, more attention should be paid to caring for transgender individuals (Flores et al., 2016). This case study explores barriers trans- gender people may face in health care along with nursing care consid- erations.
Case Description Andrew, a 48-year-old male, enters an emergency room (ER) with a fever. The receptionist asks for the patient’s driver’s license to begin the admission process. Immediately the receptionist no tices a discrepancy between the patient’s name, physi- cal appearance, and gender listed on the license. The driver’s license iden- tifies a person named Anna as a Caucasian female with long blonde hair and no facial hair. Andrew is bald and has facial hair. The recep- tionist says, “Excuse me. I noticed a discrepancy with your appearance and the picture on the driver’s license. Do you have another form of ID?” Andrew explains he is a transgender male. He states he never
Case Study
Transgender people face potential healthcare barriers, including communication issues, violations to HIPAA, inappropriate room assignments, and failure of standards of care. Appropriate nursing care considerations for transgender patients are explored.
updated his driver’s license because he never had time. The receptionist replies, “Thank you for the clarifica- tion.”
A few minutes later, the triage nurse comes out to the waiting area and asks for “Anna.” As the nurse repeats the name a couple of times, Andrew realizes the nurse was call- ing for him. He reluctantly stands up and follows the nurse into the triage room. Chatter and some laughs are heard among people in the waiting room. The receptionist pulls the nurse aside. Outside the room, Andrew can listen to the receptionist tell the nurse the patient is a transgender male. The triage nurse reenters the room and immediately apologizes. Andrew accepts her apology but states, “I am a man. Please use male pronouns.”
With the admission completed, the nurse asks if she can place Andrew in a cohort ER male room temporarily, as all the private rooms are taken at the moment. He states that is fine. She prints his identifica- tion bracelet with his legal name and walks him to his ER room. The triage nurse gives bedside report to the ER nurse, informs her Andrew is a transgender male, and asks her to refer to him using male pronouns.
The ER nurse conducts a head-to- toe assessment, assesses the pa tient’s vital signs, and confirms Andrew is in atrial fibrillation after an EKG. The ER nurse reports to the ER physician that Andrew is a 48-year- old transgender male with a fever and burning on urination. She dele- gates to her nursing assistant the collection of a urine sample for uri- nalysis, urine culture, and urine human chorionic gonadotropin test from Andrew. A couple of minutes later, the nursing assistant hands Andrew a urinal and requests a urine sample. Embarrassed, Andrew tells her he needs a collection hat for his urine. The nursing assistant be – comes confused and asks why. Andrews explains he’s a transgender male. The nursing assistant, still con fused, asks if he has a penis. Andrew again requests a hat. The nursing assistant confronts the ER nurse at the nursing station and asked why she didn’t tell her the patient is “passing off as a guy.” The ER nurse quickly apologizes in embarrassment and says she forgot. A hospital custodian overhears the conversation and asks the nursing assistant if the patient was gay. The nursing assistant says she doesn’t know but he’s transgender.
July-August 2020 • Vol. 29/No. 4238
The ER physician assesses Andrew and explains he might have a uri- nary tract infection (UTI) due to being biologically born female. Andrew interrupts the physician, saying he was assigned female at birth. The ER physician is taken aback and apologizes. He continues to assess Andrew. During the assess- ment, Andrew redirects his eye con- tact past the ER physician. The ER physician turns around to find the roommate peeking through the cur- tains. The ER physician asks the roommate to excuse them, as they’re having a private conversation. The roommate awkwardly returns to his bed. The physician finishes the con- versation and goes to admit Andrew due to a possible UTI and atrial fibril- lation.
The ER nurse informs Andrew he will be admitted to the cardiac telemetry unit. She notes a private room may not be available and asks if he would like to share a room with another male patient. Andrew indi- cates he would rather have a private room. The nurse informs Andrew he might be held in the ER until a pri- vate room is made available. Andrew agrees and asks the nurse to excuse him as he will use the men’s rest- room to get the urine specimen.
After the conversation with the ER nurse, Andrew’s roommate asks to speak with the charge nurse. The charge nurse walks into the room and the roommate demands to change his roommate because he refuses to share a room with a “she- male.” Andrew returns to his room and the charge nurse tells him his bed has to be moved into the hall- way. He asks why and the charge nurse redirects the conversation by stating they’re trying to find him a private ER room. Seven hours later, Andrew is still on a stretcher in the hallway. The ER nurse tells him he is being transported to the cardiac telemetry unit.
Andrew is transported to his new private room on the cardiac teleme- try unit. The ER nurse gives bedside report to the unit nurse and explains Andrew is a transgender male. The nurse welcomes Andrew to the unit and takes his vital signs. As the
nurse continues her assessment, she explains she has to apply a heart monitor to assess the patient’s atrial fibrillation continuously. As the nurse prepares to apply the heart monitor, she notices the patient is wearing a chest binder. She asks him to remove the chest binder, but Andrew states he would rather not. Confused, the nurse asks why he is wearing it. Andrew says it is to flat- ten his chest so people do not mis- take him for being female. The nurse apologizes but explains the chest binder interferes with applica- tion of the electrodes and will dis- rupt cardiac monitoring. Andrew agrees to remove the chest binder.
As the nurse completes her assess- ment, Andrew asks if he can use a razor to shave his head for the morning. The nurse recommends avoiding all razors because he is tak- ing an anticoagulant and could bleed excessively if he cut himself. Andrew then asks if he could use makeup; the nurse agrees, stating this is not against hospital policies.
An hour later, a phlebotomist enters the room and explains she will take some blood for laboratory testing. She asks the patient to state his name and date of birth; he iden- tifies his birth date and indicates his name is Andrew. The phlebotomist reverifies his name band, which does not match with his stated name. Andrew realizes his name band has his legal name, explains he has not changed his name legally, and pro- vides the phlebotomist with his dri- ver’s license. The phlebotomist rever- ifies the name but is taken aback by the different appearance of the pic- ture in his license. She asks the patient’s nurse to verify she is taking blood from the correct patient. The nurse assures the phlebotomist that this is the correct patient.
After 3 days in the hospital, Andrew has no more fevers and reports reduced burning with urina- tion. He is discharged home with a prescription for antibiotics.
Discussion Lambda Legal (2016) cited possi-
ble challenges to transgender pat –
ients, including inappropriate be – havior, violations of the Health Insurance Portability and Accounta – bility Act (HIPPA), improper use of name and pronouns, inappropriate questioning, challenges in bath- room use, inadequate room assign- ments, and failure of standards of care. This case study explored differ- ent issues possibly experienced by transgender patients in the hospital. One of the biggest problems Andrew faced was inappropriate communi- cation and interaction. The 2015 U.S. Transgender Survey found 24% of 27,715 respondents reported hav- ing to educate their healthcare providers on transgender people (James et al., 2016). In the case study, for example, the nursing assistant did not understand the meaning of transgender male. If a staff member does not understand the meaning of transgender, he or she should ask the patient. However, all nurses should remember all ques- tions should be related to the patient’s health and should be nonabrasive and nonjudgmental. Additionally, nurses and all health- care professionals should become educated in use of a few common terms in transgender culture to avoid misconceptions (see Table 1).
Another barrier unique to trans- gender persons is proper identifica- tion. The discrepancy with Andrew’s license is common; only 11% of the 27,715 respondents of the 2015 U.S. Transgender Survey had their pre- ferred name and gender on all iden- tification (James et al., 2016). Quest – ioning the discrepancy is appropri- ate, as the receptionist and phle- botomist did. Still, admission forms and identification bracelets should include an option of gender identifi- cation and preferred names, respec- tively, to prevent discrepancies. Lambda Legal (2016) suggested hos- pital staff could ask gender identity and sex assigned-at-birth as part of the admission profile. Adding an optional field for nicknames and pronouns also would help commu- nication for transgender patients. This may be a common occurrence for transgender people. According to Lambda Legal, transgender patients should be addressed using names or
Case Study
July-August 2020 • Vol. 29/No. 4 239
Room Assignments, Gender Identity, and Gender Expression: A Case Study on Caring for Transgender Patients
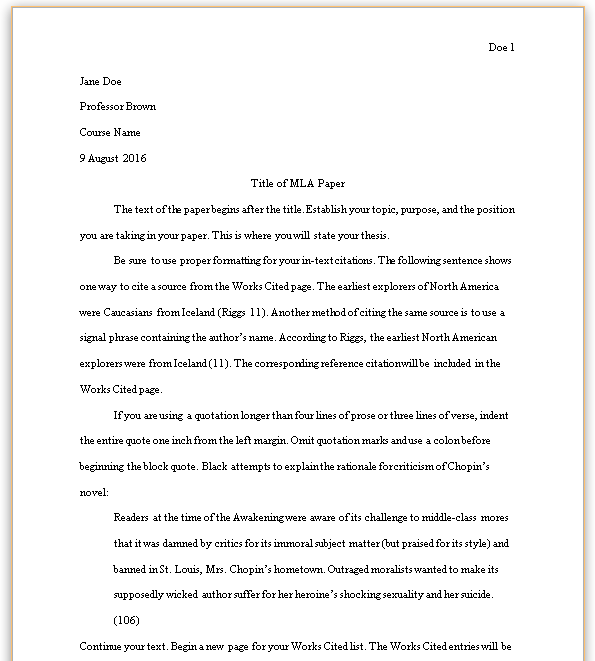
TABLE 1. Glossary of Transgender Terms
Term Definition
Sex Classification of a person as male or female based on appearance of external anatomy
A person’s sex is determined by chromosomes, hormones, internal and external reproductive organs, and secondary sex characteristics.
Gender Identity Personal sense of one’s own gender
Gender identity may not always match the sex assigned at birth. People may identify themselves as man, woman, or non-binary.
Gender Expression External manifestation of a gender
This is embodied by a person’s name, pronouns, clothing, haircut, behavior, voice, and body characteristics. Gender expression can be described as masculine or feminine.
Sexual Orientation Person’s physical, emotional, or romantic attraction to another person.
Terms straight, gay, lesbian, bisexual, and queer describe a person’s sexual orientation.
Transgender Umbrella term when sex is different from a person’s gender identity or gender expression
The terms female, male, woman, or man following transgender usually describes the gender identity or expression. Transsexual is an older term used to describe people undergoing transition through medical interventions (surgical or medical).
Cisgender Describes people who are not transgender
Non-binary or Genderqueer
Used by those whose gender identity or gender expression is not categorized as male or female
Transition Change over time from one gender to another
Transition may include coming out, using a different name or pronouns, change in gender expression or identity, hormone therapy, and surgery.
Source: Gay & Lesbian Alliance Against Defamation, 2016
TABLE 2. Words and Phrases to Avoid
Avoid Preferred Rationale
Transgenders or a transgender
Transgender people or a transgender person
Transgender is used properly as an adjective to describe a person, not as a noun.
Transgenderism Being transgender Transgenderism often has a negative connotation. It may be used by anti-transgender activists to describe being transgender as a condition.
Biologically/genetically born male/female
Assigned male/female at birth Using the term biologically or genetically undermines a person’s gender identity.
Sex change Transition This phrase produces the incorrect impression that surgery is required for a transgender person to transition.
Passing/posing/pretend – ing as male/female
Visibly/not visibly transgender Using the phrase passing as may imply inauthenticity (being something other than the person is). Transgender people live their gender identity as authentic.
Tranny, she-male, he-she, it, and shim
Use the person’s preferred name and pronoun.
Many transgender people find these terms offensive and dehumanizing. Use their names and ask them what pronoun is appropriate to use.
Source: Gay & Lesbian Alliance Against Defamation, 2016
July-August 2020 • Vol. 29/No. 4240
Case Study
pronouns they deem appropriate. In the case study, Andrew overheard the receptionist and the emergency physician using the wrong pronoun. Using phrases such as biologically born female and passing as a male can be offensive as they undermine a person’s gender identity. See Table 2 for examples of terms to avoid and words preferred by a transgender person.
Lack of communication between staff in the case study created awk- ward encounters for the patient. For example, the ER nurse called for Anna instead of Andrew in a room full of people. This attracted atten- tion in the waiting area because Andrew’s gender identity did not match Anna’s feminine name. Sharing information of patients with other personnel is also inap- propriate and a violation of HIPAA, affecting the patient’s right to priva- cy and confidentiality (Lambda Legal, 2016). Andrew’s nursing assis- tant told a hospital custodian, who was not involved with patient care, that he is a transgender male. According to Lambda Legal, “Pri – vacy can be especially important to transgender patients who may not want their transgender status dis-
closed for personal or safety rea- sons” (p. 6).
Transgender people have the right to receive care without dis- crimination or harassment due to gender identity or expression (Lambda Legal, 2016). According to James and coauthors (2016), 6% of over 27,000 surveyed transgender people reported being abused ver- bally in a healthcare setting. In one account by Hanneman (2017), an anonymous transgender male stated the doctor kept referring to him as she in front of other staff members despite correcting him multiple times. Samuels and colleagues (2015) reported numerous transgen- der participants in their study feel- ing “like a freak show” (p. 174). In Andrew’s situation, the ER nurse was right to separate Andrew from the roommate who used inappropriate language and slurs. However, it may have been more appropriate to con- sider both patients’ accommodation preferences rather than move Andrew first.
Per the Patient Protection and Affordable Care Act, hospitals are to provide equal access to their health programs or activities without dis- crimination based on sex (Romero,
2016). Lambda Legal (2016) estab- lished seven guidelines in order of priority on how to assign rooms for transgender patients (see Table 3). In the case study, the ER nurse first should have given Andrew the option of a private room, or a semi- private room shared with a patient of his identified gender. This was addressed by offering a private room when he was admitted to the car- diac telemetry unit.
After arriving at the unit, Andrew faced issues with gender expression. This included use of a chest binder, boxers, razor, makeup or personal belongings that assist with gender presentation. Lambda Legal (2016) indicated bringing personal belong- ings does not apply to items that can jeopardize a patient’s health. Additionally, hospital policies may differ with patient access to personal belongings. In this instance, the nurse allowed the use of makeup as it was not against hospital policy. The nurse could have suggested using an electric shaver as an alter- native to using a razor blade. Finally, the nurse explained how a chest binder might interfere with the
TABLE 3. Room Assignment Policy for Transgender Patients
1. If a transgender patient requests to be assigned to a room with a roommate of the patient’s same gender identity and such a room is available, the request should be honored.
2. If a transgender patient requests a private room and there is one available, it should be made available to the patient.
3. If a transgender patient does not indicate a rooming preference and a private room is available, the private room should be offered to the transgender patient. The offer should be explained to the patient as optional and for the purpose of ensuring the patient’s privacy, safety, and comfort.
4. If a private room is not available and the transgender patient does not wish to share a room with a roommate, the transgender patient should be assigned to an empty double room with the second bed blocked.
5. If there is no private room or empty double room available, the patient should be assigned to a room with a patient of the gender with which the transgender patient identifies.
6. If there is no private or empty double room available and a transgender patient does not wish to share a room, other patients may be moved to make a private room available if doing so would not compromise the health or safety of the patients being moved.
7. If there is no private or empty double room available, the transgender patient refuses to share a room, and no other patient can safely be moved to make a private room available, the transgender patient should be allowed to remain in the Emergency Department or Admitting Office without harassment until a private room becomes available.
Source: Lambda Legal, 2016
continued on page 244
July-August 2020 • Vol. 29/No. 4244
telemetry monitor. Allowing patient access to personal belongings that assist with gender expression helps create a more therapeutic environ- ment for them.
Conclusion Education, communication, and
respect are keys to creating a healing environment for transgender pa – tients. Andrew had several health- care experiences that may be com- mon to some transgender patients. Nurses and other healthcare profes- sionals should be educated about use of appropriate terms and com- munication strategies for interacting with transgender patients. This in – cludes using correct pronouns and proper identification as indicated by the patient. Nurses must respect their patients’ privacy and advocate for their right to be cared for in a nondiscriminatory, harassment-free environment. Finally, nurses must create an environment that allows gender expression for transgender patients. Hopefully, these nursing care interventions will reduce barri- ers transgender people may face in health care and provide better out- comes.
REFERENCES Gay & Lesbian Alliance Against Defamation.
(2016). GLAAD media reference guide – transgender. https://www.glaad.org/refer ence/transgender
Hanneman, T. (2017). Healthcare equality index 2017. https://assets2.hrc.org/files/ assets/resources/HEI-2017.pdf?_ga= 2.252954889.1065832987.1586066083 -187025126.1586066083
Flores, A.R., Herman, J.L., Gates, G.J., Brown, & Taylor, B. (2016). How many adults identify as transgender in the United States? https://williamsinstitute. law.ucla.edu/publications/trans-adults- united-states/
James, S.E., Herman, J.L., Rankin, S., Keisling, M., Mottet, L., & Anafi, M. (2016). The report of the 2015 U.S. Transgender Survey. https://www.trans equality.org/sites/default/files/docs/ USTS-Full-Report-FINAL.PDF
Lambda Legal. (2016). Creating equal access to quality health care for transgender patients. https://www.lambdalegal.org/ sites/default/files/publications/down loads/fs_20160525_transgender-affirm ing-hospital-policies.pdf
Romero, A.P. (2016). Nondiscrimination in health programs and activities: Pro posed rule RIN 0945-AA02. http://federal register.gov/a/2016-11458
Samuels, E.A., Tape, C., Garber, N., Bowman, S., & Choo, E.K. (2015). “Sometimes you feel like the freak show:” A qualitative assessment of emergency care experiences among transgender and gender-nonconforming patients. Annals of Emergency Medi – cine, 71(2), 170-182.e1. https://doi.org/ 10.1016/j.annemergmed.2017.05.002
Case Study continued from page 240
Copyright of MEDSURG Nursing is the property of Jannetti Publications, Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder’s express written permission. However, users may print, download, or email articles for individual use.